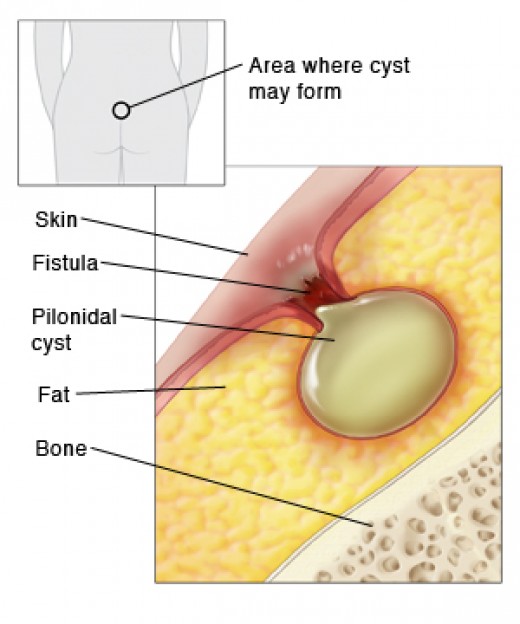
Pilonidal Cyst
A pilonidal cyst is an abnormal pocket in the skin that usually contains hair and skin debris. A pilonidal cyst is almost always located near the tailbone at the top of the cleft of the buttocks. Pilonidal cysts usually occur when hair punctures the skin and then becomes embedded. If a pilonidal cyst becomes infected, the resulting abscess is often extremely painful. The cyst can be drained through a small incision or removed surgically. Pilonidal cysts most commonly occur in young men, and the problem has a tendency to recur. People who sit for prolonged periods of time, such as truck drivers, are at higher risk of developing a pilonidal cyst.
Symptoms
When it’s infected, a pilonidal cyst becomes a swollen mass (abscess). Signs and symptoms of an infected pilonidal cyst include:
- Pain
- Reddening of the skin
- Drainage of pus or blood from an opening in the skin
- Foul smell from draining pus
When to see a doctor
If you notice any signs or symptoms of a pilonidal cyst, see your doctor. He or she can diagnose the condition by examining the lesion.
Causes
The exact cause of pilonidal cysts isn’t clear. But most pilonidal cysts appear to be caused by loose hairs that penetrate the skin. Friction and pressure — skin rubbing against skin, tight clothing, bicycling, long periods of sitting or similar factors — force the hair down into skin. Responding to the hair as a foreign substance, the body creates a cyst around the hair. This explanation accounts for rare cases of pilonidal cysts that occur in parts of the body other than near the tailbone. For example, barbers, dog groomers and sheep shearers have developed pilonidal cysts in the skin between fingers.
Risk factors
Certain factors can make you more susceptible to developing pilonidal cysts, such as:
- Male sex
- Younger age (pilonidal cysts are most common in people in their 20s)
- Obesity
- Inactive lifestyle
- Occupation requiring prolonged sitting
- Excess body hair
- Stiff or coarse hair
Complications
If a chronically infected pilonidal cyst isn’t treated properly, you may be at slightly increased risk of developing a type of skin cancer called squamous cell carcinoma.
Surgery
The surgical treatment is to remove the entire cyst down to healthy tissue. Electrocautery is used to dissect the tissues toward the sacrum around the cyst and sinus tracts. Dissection is performed in healthy tissue approximately 0.2 cm lateral to the identified sinus tracts. For small cysts, dissection can continue above the cyst and from both sides. In larger cysts, dissection is continued until the fascia overlying the sacrum is encountered, but the fascia is left intact. Occasionally, the walls of the wound are debrided further with curettage. Hemostasis is maintained with electrocautery. After a cystectomy with no tension on the skin edges, the wound is closed multiple in layers using absorbable sutures. The skin is then closed with sutures and a bolster is used to reduce tension on the suture line. This is an outpatient surgery. The bolster comes off in 3 days, half the skin sutures come out at two weeks, and the other half come out in three weeks. Typical recovery time is 3-6 weeks.